Introduction
The New Hampshire Charitable Foundation, in partnership with the partnership with the Conrad N. Hilton Foundation, launched the NH Youth S·BI·RT Initiative beginning in January 2014 and continuing through June 2017. The NH Youth S·BI·RT Initiative aimed to support the adoption of S·BI·RT as a sustainable and universal practice in New Hampshire by addressing the following goals:
- Expand youth S·BI·RT in primary care settings;
- Screen no less than 10,000 youth and young adults (age 12-22) by 2017; and
- Address policy and financial barriers that were identified during the project.
The NH Center for Excellence at the Community Health Institute provided technical assistance to grantees. New Futures provided policy and advocacy support to address identified legislative or regulatory barriers.
The New Hampshire Charitable Foundation invited proposals, ultimately funding three cohorts of practice sites over the three and a half year period (2014-2017) of this project. Funding covered S·BI·RT implementation expenses such as staff planning and training time, and modifications to electronic medical record systems. Each funded practice site formed a team that included a medical champion, a behavioral health specialist, an information systems expert and a member with authority to make decisions, such as a medical director of administrator.
The project was structured as an action learning collaborative, engaging teams from the different clinical practice sites in shared learning and supporting sustainable system-based methods of quality improvement. Facilitation of S·BI·RT implementation included training, technical assistance, and the development of a range of resources to support the process at the practice level.
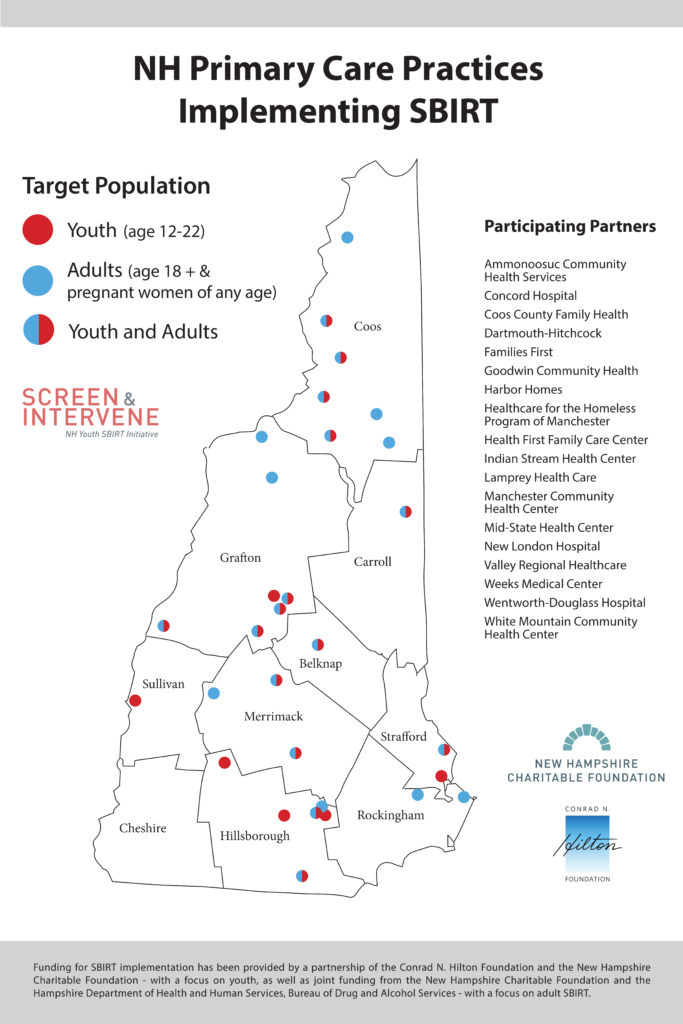
Ten organizations across 23 practice sites, collectively serving over 74,000 patients ages 12-22, included a range of rural and urban service delivery settings, including Federally Qualified Health Centers and other community health centers, a large academic healthcare system, a mid-sized healthcare system, and two critical access hospitals. Several of the practices were patient-centered medical homes.
Implementing Practice Sites
- Concord Hospital Family Health Centers
- Dartmouth-Hitchcock Medical Center – OB/GYN Lebanon, Pediatrics – Lebanon, Plymouth, Bedford, and Manchester
- Goodwin Community Health Center
- Health First Family Health Center
- Manchester Community Health Center
- Mid-State Health Center
- Valley Regional Hospital Wentworth-Douglass Hospital
- Weeks Medical Center
- White Mountain Community Health Center
The Initiative screened 15, 126 youth, and provided training to nearly 600 providers and other ancillary staff
77% of youth seen in primary care for routine visits were screened using a validated screening tool.
- Of those screened, 15% were found to be at risk for a substance use
- Of youth found to be at risk
- 41% received a brief intervention (6% of all youth screened) and
- 28% were at sufficient risk to need a referral to
 behavioral health services for further assessment and treatment (5% of all youth screened)
behavioral health services for further assessment and treatment (5% of all youth screened)
- 70% of practice sites developed partnerships with other organizations
Key Lessons Learned
Key lessons learned by working closely with the implem
enting practice sites, fell into three broad categories.
I. S·BI·RT implementation requires a meaningful investment of time, effort, and resources devoted to addressing technical operations as well as practice culture. Keys to success include:
- Strong support from leadership;
- A medical provider champion to promote the SBIRT implementation among peer providers and set performance expectations;
- Time dedicated to meetings and QI related to work-flow and roles; and
- A robust information technology department working with implementation and QI efforts.
II. The EMR plays a critical role in S·BI·RT to support and document clinical
III. There are broader implications for policy that include barriers related to billing and coding of screening as a reimbursable service, and confidentiality considerations related to patient care, as well as organizational compliance with federal and state regulations.
The Initiative has raised awareness and understanding of S·BI·RT as a mechanism for integrating primary care and BH, and also as a prevention strategy in the face of the opioid epidemic. There is an increasing awareness of the importance of S·BI·RT throughout the state — in part a reaction to the opioid crisis, but also in part due to an increased understanding that implementing S·BI·RT is doable, that peers have adopted it successfully, and that there is expertise available through the Center.
As health systems move increasingly toward integration of primary care and behavioral health, medical professionals equipped with screening and intervention skills and best practice tools are well positioned to participate successfully, improving patient outcomes and reducing health care costs.
A detailed compilation of lessons learned and recommendations for SBIRT implementation is available in Preventing Youth Substance Misuse Through Integrated Primary Care: Strategies for SBIRT Implementation. Download the full document (PDF) or request a hard copy.
